The coronavirus as a yardstick of global health policy
Theme1
Global health is one of the few policy areas that can be considered to have been internationalised. Although it remains under construction, it already features many of the distinctive elements of a public policy. Now it faces the challenge of COVID-19, which has been officially classified as a global pandemic.
Summary
The World Health Organisation (WHO) has just declared the COVID-19 coronavirus a global pandemic . It is the latest in a series of pandemics that have appeared over the course of recent decades with worldwide repercussions for health. Awareness of pandemics goes back two centuries, but the advances in health systems, new treatments and preventive measures created the illusion that they had been eradicated. However, the appearance of new pathogens and the reappearance of others thought to have been controlled, combined with the multiplier effect of globalisation, have aggravated their impact not only as a problem of worldwide health but also as a problem of international security.
To deal with pandemics there is a global security system and policy that already possesses the elements appropriate to a public policy, such as institutions, norms, instruments and a model of global governance, which has moved from taking reactive, exceptional and case-by-case measures (securitisation) to becoming a more preventive and systematic model of response (medicalisation). As with all policies under construction, the progress made by global health policy depends on the priority it possesses on domestic and international agendas, a priority that acquires fresh urgency with each new pandemic and gets forgotten whenever society’s attention wanes. This paper analyses how the COVID-19 coronavirus has put global health policy to the test once again.
Analysis
Concern about the cholera epidemics that swept through Europe in the 19th century led to the first International Health Conference in Paris in 1851. The subsequent conferences and conventions constituted the first international response mechanism.2 They were followed by the International Office of Public Hygiene in 1907, the Health Organisation of the League of Nations in 1926 and the UN’s World Health Organisation in 1946. These institutional advances led to the approval of the first strategy of worldwide scope, ‘Health for All’, which, among other aims, sought to foster the capability to manage contagious diseases in all countries by the year 2000. This was adopted by the International Conference on Primary Health Care held in Alma-Ata in 1978.
Other multilateral and regional organisations and groupings limited to particular countries have included global health issues on their agendas and have developed mechanisms for responding.3 The first global regulatory instruments were unveiled in 1959 and have been reviewed on successive occasions since, culminating in the present International Health Regulations (IHR). These instruments have broadened and deepened international cooperation to new states and to new arenas of response. The pandemic concept has been widened to reflect its greater international impact and the obligations and capabilities required of states to shoulder their share of global responsibility have been increased. The system, organised around the WHO, has been completed with action protocols, compulsory procedures for notifying outbreaks and a Global Public Health Intelligence Network (GPHIN).
Like other instruments of international law, health regulations face the problems of interpretation stemming from the differences of criteria that exist among states; they also take time to adapt to new developments and, above all, lack the means to ensure compliance (enforcement). On the other hand, owing to the complexity and difficulty inherent in decisions dealing with pandemics (certifying outbreaks, imposing quarantines, limiting free movement…), national governments tend to base their decisions on the recommendations of the WHO and national health authorities, a de facto subordination that enhances the global health system’s scope for influence with each new outbreak. As well as the difficulties mentioned above, the construction of the global health policy has to face tangible challenges, such as the proliferation of new pathogens and the exponential speed at which they spread, owing to global mobility and connectivity, and intangible challenges, such as the loss of institutions’ credibility and the social alarm spread through the Internet and social media.
Despite all this, the global health system now possesses a remarkable store of experience. In addition to the emergence of HIV/AIDS and the endurance of such intractable pathogens as those responsible for malaria and meningitis there have been new pathogens triggering haemorrhagic fevers in Africa, bovine spongiform encephalopathy in Europe as well as the West Nile and Nipah viruses, originating in the Nile Delta and Malaysia respectively. With the advent of the 21st century, global health has faced new pandemics of which six have been declared by the WHO as Public Health Emergencies of International Concern since the entry into effect of the WHO’s International Health Regulation of 2005: the 2009 flu pandemic (Influenza A), wild poliovurus and Ebola in 2014, the Zika virus in 2016, Ebola in 2019 and COVID-19 in 2020.
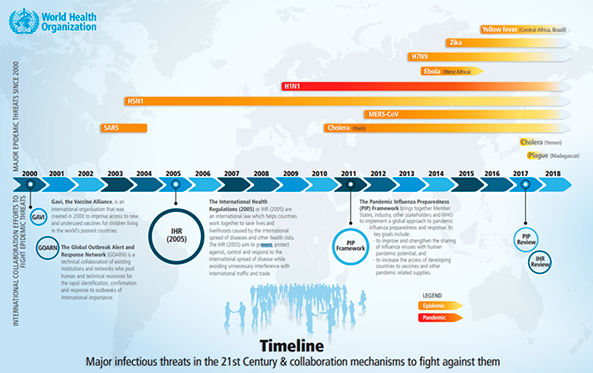
Each pandemic has had its own impact, determined by its particular characteristics of lethality, the populations affected and the media impact, which in turn has helped the lesson-learning process.4
It is possible to draw certain conclusions from the lessons learnt regarding the way global health policy works. The first is that the expectations of a global and connected society regarding the efficacy and speed of measures exceed the actual ability of the system to respond. For one thing, the headway made by public health policies has increased the public’s level of demands and undermined their ability to accept the limits of the system. They expect new pandemics to be dealt with as effectively and rapidly as other diseases. The collective hyper-awareness fails to appreciate that preventive plans and measures count for little if a novel type of virus emerges, as in the case of the COVID-19 coronavirus. Each new pandemic requires its own learning curve to unfold and experiences like avian flu show that taking inappropriate or disproportionate steps under pressure may engender distrust in the global health system.5 The adoption of drastic measures unsupported by scientific evidence generates counterproductive effects, so that health authorities must maximise their precautions, even when verifying the existence of an outbreak, because the very act of certifying pandemic outbreaks generates widespread alarm and has irreversible economic costs for the countries involved in the health scare.
Added to the technical difficulties of managing pandemics is the difficulty of devising strategic communication. The 2009 flu crisis and the 2014 Ebola crisis revealed the growing importance of the new digital social media in the way pandemics are perceived. Reliance on media other than the official and traditional communication channels lessened the effect of the official strategic communication and, as a consequence, led to a fragmentation of public opinion towards the response measures. It did not take long for the inevitable rumours about political conspiracies, speculation and doom-mongering that swirl around social media to be joined by fake news and disinformation, as evident in the case of the COVID-19 coronavirus.6
Pandemics as a problem of international security
Pandemics were initially dealt with as problems that affected only health and their management was left, in functional terms, to health authorities and, in geographical terms, to the countries most closely concerned. This approach prevailed, with minor variations, until the new wave of pandemics mentioned above meant that the problem went from being one of health to one of security. The urgency of the problem has increased owing to the growth of transport and connectivity, climate change, urbanisation and similar factors linked to globalisation. The change of approach became necessary when the evidence revealed that pandemics were crossing national borders and inflicting collateral damage on policy areas and interests other than health. Phenomena such as AIDS served to accelerate the change of approach and ultimately it was treated as a matter of international security at the United Nations Security Council in January 2000. Treating pandemics as a security problem does not mean treating them as a military problem, an error that might have been committed in a strategic environment dominated by the September 11 attacks, the fight against terror and the risk of non-state actors carrying out attacks with infectious agents or with weapons of mass destruction for terrorist or any other type of purpose.
Consequently, the national security strategies of the new century did not include pandemics stemming from the possible use of infectious agents as weapons of war but rather due to their impact –by now notorious– on the security and prosperity of countries and due to their now being treated as problems of international security. In the case of the US, the 2002 National Security Strategy included the HIV/AIDS pandemic among the risks to be considered, as did the subsequent strategies, including the most recent in 2017; ultimately this was superseded by a broader concept of global health, for which a dedicated Global Health Security Strategy was drawn up in 2019. In its new global approach, the US strategy now seeks to focus on the external sources of epidemics (developing the capabilities of third parties) and on their internal consequences (strengthening the system of emergencies), in line with the National Security and National Biodefence Strategies, and in cooperation with other countries, organisations and non-state actors.
The switch from a reactive to a more preventative approach stems from a firm conviction that pandemics will continue to emerge. In February 2018 the Director General of the WHO, Tedros Adhanom, told an audience at the World Government Summit in Dubai that a devastating epidemic capable of killing millions of individuals could strike any country at any time, an opinion endorsed in October of the same year by a group of experts meeting at the Centre for Security and International Studies (CSIS) in Washington to assess the impact of a pandemic such as the one that has just been declared. One year later, the outbreak of COVID-19 has vindicated them and shown the need to get used to living with pandemics.
Underlying the management of pandemics is an intellectual debate about the nature and desirability of the response measures. A distinction is drawn between taking extreme, one-off and reactive measures (securitisation) and taking preventive and sustainable measures capable of offsetting the impact of pandemics and improving the resilience of health systems (medicalisation). The theoretical debate is interesting inasmuch as it supports a global health policy that rests on robust national health systems deploying capabilities for combatting pandemics (national authorities, strategies, plans, systems and measures) in coordination with the global health system described above.
Another aspect of the debate concerns the degree of sovereignty states possess to adopt measures whose causes and effects cross borders and need to be coordinated with a global system of governance. The states, and their health systems, still retain control over health competences and, for example, are the only entities authorised to certify outbreaks, even if the WHO detects them at the states’ ‘request’. However, they have to coordinate the way these competences are discharged and the measures taken with the global health system, such that while they continue being strategic actors in the management of pandemics, they are no longer the only ones. The influence of the WHO system and public health procedures is growing both over strong national systems, owing to its ability to justify the decisions they take and, above all, over weaker national systems that depend on global capabilities and resources to manage epidemics.
The efficacy of the measures
Since it is not a question of whether a pandemic will occur, but rather when and how, networks have been set up for the monitoring of contagious diseases in order to streamline the activation of response plans. The WHO combines the GPHIN communications network mentioned above with an alert and response system (GOARN) specialising in epidemic outbreaks. Both networks work in partnership with other governmental and non-governmental networks, with varying levels of resources and specialisation, and support the initiatives of governments affected by pandemics, especially those that do not have or have not provided the appropriate means to identify infectious outbreaks.
The existence of surveillance networks has considerably improved the global capacity to respond to pandemics, although empirical confirmation of such a correlation is not yet forthcoming. Moreover, in countries whose governments have fewer resources to work with, the improvement of surveillance relies on non-official networks, and while time is gained in the identification of outbreaks, it may continue to be lost in terms of the official certification or the activation of response procedures, meaning that its efficacy is limited.13
The true efficacy of global and national health systems and their capacity for resilience depends on the capabilities that they can call on, both in generic terms for overall public health and specifically devoted to pandemics. This accounts for the need to strengthen the capabilities of the weakest links in the chains of transmission of the pandemics, not only to contain the pandemics in their places of origin but also to alleviate the impact on the local populations. This dimension of health assistance to third countries in need is a key part of the new global health policies.
Although indicators have their limitations, as a means of objectively gauging performance, the Global Health Security Index affords an approximation of the security and capabilities of national systems. It includes data for the 195 states that have signed up to the International Health Regulations mentioned above. In its 2019 report,14 the overall assessment of the GHS Index states that no country is completely prepared to deal with epidemics or pandemics, and all exhibit some form of vulnerability. Scores for the various components of the Index confirm the systemic weakness: the overall average score for national health systems is 40.2 out of 100, with 115 high- and middle-income countries failing to score over 50 points. Even among the small group of countries with higher ratings, the data are far from satisfactory: only 7% of countries have a high ability to prevent the emergence or release of pathogens, only 19% receive the top score for detection and reporting, less than 5% score highly for their ability to respond rapidly and just 23% score highly for government effectiveness.
Its recommendations include measuring and publishing evaluations of health systems, improving coordination between domestic and international actors and investing in resources and financing mechanisms. On the global stage, it proposes creating the role of a facilitator reporting to the general secretary of the United Nations to coordinate responses to large-scale pandemics and run simulations of major crises. These measures are difficult to implement and those relating in particular to financing prompt a final reflection. It is estimated that an annual investment of around US$4.5 billion is needed to reduce the global lack of preparation capabilities. The investment required, while large, especially for low-income countries, would be outweighed by the economic damage caused by various epidemics and pandemics, which is estimated at around US$570 billion per year.15
Conclusions
The existence of a highly-aware and hyperconnected global society facing the prospect of epidemics and pandemics could aid the construction of a global health policy if its impetus is sustained over time. If the social and political pressure for measures to be taken wanes or is not maintained during the monitoring and execution phase, national and international health systems will refuse to engage in a more transformational agenda for global health.
Global health policy reflects the growing interdependence between national and international systems and policies. This interdependence will intensify with the persistence of pandemics, which will reduce the autonomy that health systems have enjoyed up till now.
The security focus of global health policy helps to improve international cooperation in the face of successive crises, but its efficacy ultimately rests on improvements in national response capabilities. Given that we need to learn to live with epidemics and pandemics, rather than being viewed as extraordinary, as they are at present, the measures need to become normalised and sustained over time.
Lastly, in light of the overriding importance to international security, international cooperation will need to be strengthened in order to offer financial and technical aid to the weakest links in the global health chain.
Félix Arteaga
Senior Analyst for Security & Defence, Elcano Royal Institute
1 A previous version of this ARI was originally published in Spanish on 18 March 2020: ‘El coronavirus como termómetro de la política de salud global’.
2 ‘A brief history of the World Health Organization’, The Lancet, vol. 360, 12/X/2012.
3 For example, the EU has set up its own agency for the prevention and control of infectious diseases (European Centre for Disease Prevention and Control, ECDC), which cooperates with the national authorities and with communities of experts in surveillance, information exchange measures and communication.
4 Juan Martínez Hernández (2016), ‘Pandemias y bioamenazas globales del siglo XXI’, ARI nr 42/2016, Elcano Royal Institute, 30/VI/2016.
5 Justo Corti Varela (2009), ‘Proteccionismo y pandemia gripal: una perspectiva española’, ARI nr 83/2009, Elcano Royal Institute, 28/V/2009.
6 The WHO has had to team up with news agencies and the major technology platforms to offset misinformation about the coronavirus.
7 Susan Peterson emphasises the way in which the then Vice-president, Al Gore, called for a new, broader definition of security that would include AIDS and other contagious diseases. ‘Epidemic disease and national security’, Security Studies, vol. 12, nr 2, 2002/3, p. 43-81.
8 Earlier than others, Bruce Hoffman explained the confluence of causes and actors that raised the prospect of weapons of mass destruction being employed. See ‘Terrorism and weapons of mass destruction’, RAND, 1999.
9 ‘United States Global Health Security Strategy’, White House, 2019; National Biodefence Strategy, White House, 2018; United States National Security Strategy, 2017.
10 Jolene Creighton quotes him as saying, ‘A devastating epidemic could start in any country at any time and kill millions of people because we are still not prepared. The world remains vulnerable’, at the World Economic Forum, 12/II/2018.
11 Samuel Brannen & Kathleen Hicks (2020), ‘We predicted a coronavirus pandemic’, Politico, 3/VII/2020.
12 Stefan Elbe (2010), ‘Pandemic Security’, in J. Peter Burgess (ed.), The Routledge Handbook of New Security Studies, Routledge, p. 163-172.
13 Sara E. Davies (2009), ‘Preparing for pandemics through surveillance’, ARI nr 9/2009, Elcano Royal Institute, 14/I/2009.
14 ‘2019 Global Health Security Index’, Johns Hopkins, The Economist and NTI.
15 ‘Harnessing multilateral financing for health Security preparedness’, CSIS, April 2019.