The COVID-19 pandemic has highlighted how social vulnerability of some groups within countries increases their risk of infection from communicable diseases; hinders access to treatment and preventive measures, including vaccination; and, overall, exposes them to worse health outcomes. Their higher exposure to communicable diseases due to social vulnerability may affect not only socially vulnerable population groups, such as migrants and refugees (M&R), but also the population at large.
G20 countries should jointly commit to develop internationally coordinated domestic policies, as well as international aid programmes, ensuring an inclusive, free-of-charge and proactive COVID-19 vaccination offer to M&R, irrespective of their legal status; and to extend this approach beyond the current pandemic and the COVID-19 vaccine, in order to reduce health inequities and enhance preparedness for present and future health threats.
Challenge
The COVID-19 pandemic is powerfully highlighting the fact that the social vulnerability of some groups within countries exposes them to higher risk of infection; to lower access to preventive and treatment measures, including vaccination; and, overall, to worse health outcomes.
In the context of the present and possible future pandemics and epidemics, this puts at risk individual and collective health, unless socially vulnerable groups have access to adequate healthcare services including vaccination. In this policy brief, we focus on the case of migrants and refugees (M&R).
M&R1 may face a higher risk of contracting communicable diseases (CDs). M&R are often exposed to various risk factors before, during and after migration, which may favour the spread of CDs: these include malnutrition, unsanitary living conditions and overcrowded accommodations. Moreover, instability and disruption of national healthcare services in their countries of origin may entail suboptimal vaccine coverage on arrival (WHO-EURO, 2018b).
Within the M&R population, some disadvantaged subgroups are at significantly higher risk of contracting a disease or of its severe consequences in areas with high transmission (WHO, 2020b). This may be due to their living conditions, which make physical distancing difficult, and/or to their legal status, which make them particularly hard to reach or may exclude them from healthcare services. These subgroups include M&R living in informal settlements or in camp-like settings, in reception centres, in prisons and restricted communities, those who are homeless, or are undocumented migrants. This pattern is very evident for COVID-19, but is also documented for other CDs, such as tuberculosis or blood-borne virus infection (WHO-EURO, 2018b).
M&R have also suboptimal vaccination coverage for vaccines recommended by WHO, compared to the general population in destination countries: clusters of unvaccinated population, such as M&R, may lead to vaccine-preventable disease (VPD) outbreaks in host countries, due to several concurrent factors (Riccardo, 2012; De Vito, 2017; Wilson, 2018; Charania, 2019; ECDC, 2021):
- Exclusion from health and vaccination plans and systems, often due to a lack of legal entitlements to health care, or to administrative/residence barriers; in some cases this exclusion is due to an open political intention to discriminate against M&R in the provision of vaccines, in others to political unawareness of consequences for individual and public health;
- Health system barriers due to, for instance, language, lack of cultural sensitivity within the health system, lack of outreach and community engagement capacity, lack of collaboration with relevant NGOs and civil society organisations; and also access barriers to primary care and vaccination services, including vaccination costs, as well as the high mobility of this population group;
- Lack of trust in the health system on the part of M&R; misconceptions about the vaccine due to misinformation or cultural beliefs.
The present situation in terms of vaccination policies for M&R together with the related data collection, monitoring and evaluation is highly heterogeneous in European (Ravensbergen, 2019) and other G20 countries.
- A pre-COVID-19 survey covering all EU and EEA (European Economic Area) countries showed that 28 out of 29 countries offer vaccination to child and adult M&R; however, seven countries limit the vaccinations offered only to adult M&R with certain conditions (such as specific health condition or country of origin). All the vaccinations included in the National Immunisation Plan appropriate for the age are offered to child and adolescent M&R in 27 countries, whereas in only 13 countries they are offered to adult M&R. Data collection methods are very heterogeneous, with only three countries reporting data on vaccination uptake among M&R. Procedures to guarantee access of M&R to vaccinations at the community level are available in 13 countries (Giambi, 2019).
- The United States includes immunisation as part of the medical examination overseas before traveling to the US among the requirements for planned migration (Mitchell, 2019Differences in migrant children’s immunisation coverage between vaccines included or not in the National Immunisation Plan in East China are attributed to the fact that the latter imply an out-of-pocket payment by caregivers, and are therefore often foregone (Hu, 2015).
- Heterogeneity with respect to M&R’s legal status clearly emerged for COVID-19 vaccination entitlement across the globe: few EU countries explicitly included undocumented migrants in their vaccination strategies (PICUM, 2021); Singapore committed to vaccinate migrant workers against COVID-19, starting with 10,000 dormitory residents (MoH, 2021); and Rwanda included refugee settlement dwellers working as community health workers, cleaners or security guards at local health clinics in the national vaccination plan (UNHCR, 2021).
Proposal
RATIONALE FOR A FULL INCLUSION OF M&R IN VACCINATION PLANS DURING AND BEYOND COVID-19
Substantial evidence shows that the rate of novel diseases emergence is increasing (Dobson, 2020). Primary prevention interventions, including vaccination, are at the core of the public health response to promote health and prevent diseases. The brief overview above shows that socially disadvantaged groups, such as M&R, are often benefitting less from those interventions. Yet, multiple elements indicate that their immediate and full inclusion in vaccination plans during and after COVID-19 is essential and should not be postponed.
1. Including M&R in vaccination programmes not only protects this group, it also protects the entire community from the risk of further outbreaks. In order to achieve national or global herd immunity, it is necessary to provide vaccination to large sections of the population, including socially disadvantaged and marginalised communities. In addition, M&R are often highly mobile and may contribute to cross-border disease spread, especially for those individuals originating from countries with limited vaccine implementation or lower vaccination coverage.
2. Improving vaccination coverage at the national and global level is considerably more effective than sustaining the economic and public health impact of controlling a disease outbreak once transmission is established and treating affected individuals, as COVID-19 shows. The global economic impact of the COVID-19 pandemic was estimated at US$ 375 billion every month in 2020 (WB, 2020); unless vaccines are distributed equitably, it will take years before COVID-19 is controlled, with adverse consequences for the recovery of the global economy.
3. Vaccination should be considered as a health equity intervention: it is crucial that action is taken to prevent the exclusion of M&R in the access to COVID-19 vaccines in order to prevent this group from bearing a disproportionate burden of the disease; COVID-19 vaccination can also offer an opportunity to favour access to care for M&R, including other vaccination and preventive services.
Universal access to available vaccinations throughout the life course is recommended for all, including M&R, on an equal footing with the local population, as affirmed also by Sustainable Development Goals (SDG) Target 3.8 “Achieve Universal Health Coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all”. Specifically, equity in the access to COVID-19 vaccines was called for by the World Health Organization (WHO, 2020a) and the European Centre for Disease Prevention and Control (ECDC, 2020), among other institutions.
ROADMAP FOR M&R INCLUSION IN PREVENTION AND VACCINATION SERVICES
For the reasons above, G20 countries should jointly commit to develop domestic policies and to ensure (including via international aid programmes) an inclusive, free-of-charge and proactive COVID-19 vaccination offer to M&R, irrespective of their legal status; and to extend this approach beyond the current pandemic and the COVID-19 vaccine, in order to reduce health inequities and enhance preparedness for present and future health threats.
Recognition by G20 leaders of the need to proactively offer vaccination to M&R would have a catalytic effect both in terms of national/international funding allocation and in terms of international consensus building, ultimately contributing to raising the issue in the global (public health) agenda. Endorsement by the G20 of an inclusive approach to COVID-19 vaccination would add political weight to the technically solid positions already developed by the WHO (WHO, 2020a), ECDC (ECDC, 2020) and other technical institutions on this issue, and consequently promote national alignment in the short and long term.
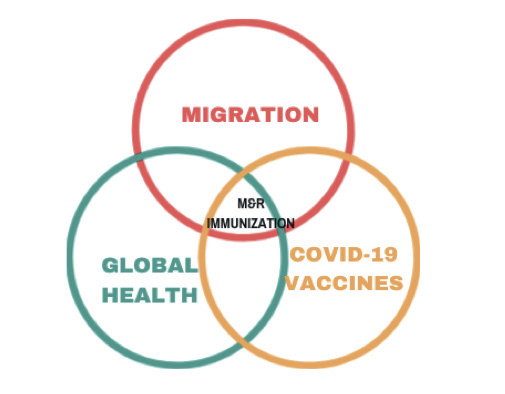
Figure 1: Inclusion of M&R in COVID-19 vaccination plans is at the interface of key G20 priorities
The COVID-19 crisis has a transformative potential in terms of prevention and vaccination approach, which should not be missed: it is vital not only that countries respond to the COVID-19 pandemic with inclusive vaccination policies, but also that this approach, presently imposed by the necessity to interrupt transmission, is transferred to the whole preventive and vaccination plans and services in the post-pandemic period, as indicated in the following roadmap (Figure 2).
Below we illustrate the key pillars for M&R’s inclusion in prevention and vaccination services -including monitoring indicators which need to be built at the national level in order to implement the above roadmap, while the concluding recommendations illustrate the role the G20 can play in bringing these pillars into the international health agenda.
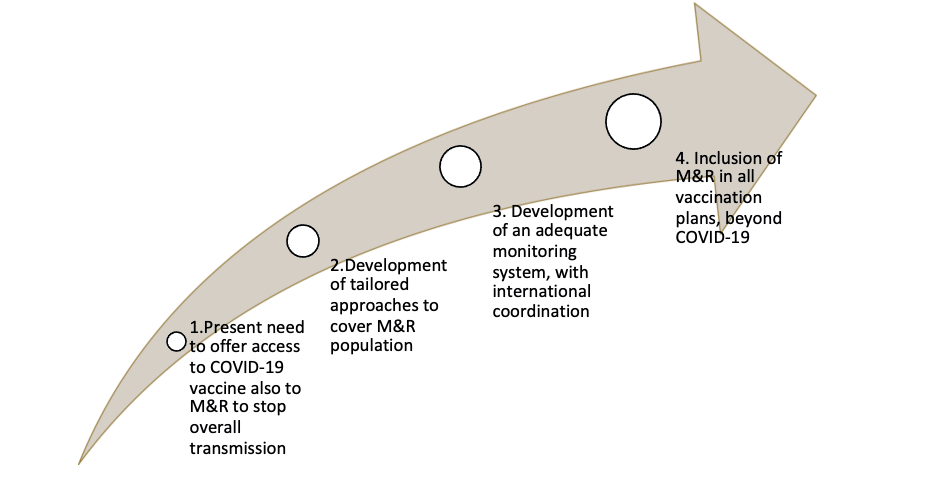
Figure 2: The roadmap towards preventive and vaccination plans and services fully inclusive of all M&R
KEY PILLARS FOR M&R INCLUSION IN PREVENTION AND VACCINATION SERVICES AND MONITORING INDICATORS
Pillar 1. Inclusion of M&R in national vaccinations plans
– Inclusion of M&R subgroups (e.g., migrants living in informal settlements or in camplike settings, in first-line and second-line reception centres, in prisons and restricted communities, as well as the homeless and undocumented migrants) among the priority groups entitled to vaccination in COVID-19 vaccination plans, with dedicated active offer strategies responding to the specific risk factors of these groups, including adequate access to reservation and registration systems as well as vaccination certificates as per national provisions.
– Inclusion of M&R in national vaccination plans beyond COVID-19, with the adoption (in terms of designing, financing, organising and evaluating) of vaccination plans extended to the entire population, including M&R regardless of their legal status or other administrative barriers.
In Italy, for example, vaccination is recommended for newly arrived M&R at the second-line reception level: children follow the national schedule, while the main vaccinations are recommended for adults (Tosti, 2020). All compulsory vaccinations are also guaranteed to undocumented migrants present in the country (Conferenza, 2012).
The Canadian Immunization Guide dedicates a full section to the immunisation of persons newly arrived in Canada, considering that they may be susceptible to vaccine-preventable diseases due to lack of effective immunisation programmes in their country of origin, and to frequent visits to friends and relatives in their home country (PHA, 2021).
Pillar 2. Development of tailored, innovative and equitable approaches for public health vaccination services targeting M&R
National and regional immunisation plans and guidelines should foresee strategies to overcome possible economic, organisational and cultural barriers that hinder M&R’s access to and/or use of vaccination services (WHO-EURO, 2019). This may include:
– Free-of-charge access to vaccination services at the point of delivery; –Strengthening health systems and primary healthcare providers, enhancing in particular the accessibility, decentralisation and outreach capacity of vaccination services, in order to reach M&R (including newly arrived) living in communities, refugee camps, reception/detention centres and prisons;
– Fostering equity in health through innovative service delivery models: set up, test and implement mobile vaccination clinics, combined healthcare services (such as antenatal care and vaccination programmes) and mass vaccination (Bartovic, 2021);
– Developing participatory approaches and engagement strategies to strengthen uptake, alongside innovative delivery mechanisms and tailored approaches to respond to specific determinants of M&R under-immunisation (Crawshaw, 2021).
For example, three health system strategies were successfully adopted in China to address barriers to immunisation for migrants: service fees charged for immunisation were discontinued; children’s immunisation certificates were checked annually and catch-up programmes organised; and local immunisation staff identified children with outdated immunisation, including migrant children (Fang, 2017).
A large worldwide literature review reports that a focus on barriers to accessing services related to language, culture, distance and cost is a key element of the most effective interventions to reduce the burden of vaccine-preventable diseases among M&R; engagement with community members and organisations was an effective way to co-design interventions to address M&R’s specific needs (Charania, 2020).
Tailored vaccination programmes in the form of mass vaccination campaigns have been developed to address gaps in vaccination coverage among M&R children in Greece. Vaccination was mainly conducted by experienced NGOs, with the support of the national health system and the Institute of Public Health. Specific mass campaigns have been organised to implement the priority vaccination programme for M&R living in all types of settings, including children living in residential centres and in other urban areas (e.g., hotels, apartments) or in atypical structures (WHO-EURO, 2018a).
Mobile vaccination teams were launched in Flanders, Belgium, in 2014, with the aim of providing free vaccination services and promoting vaccine literacy among socially disadvantaged people. These teams focused on children identified by the School Health Service or the Flanders Agency for Child and Family and provided free of-charge services to those who could not access medical care. Potential target groups included Roma, victims of trafficking, and homeless people. Vaccination data were recorded in a centralised system, and made available to all other vaccination services. Moreover, since 2016, all asylum seekers in Belgium are offered catch-up vaccinations at the time of their asylum application (WHO-EURO, 2018a).
Pillar 3. Increased staff engagement
– Increasing cultural sensitivity and competence for health personnel and the whole health system (WHO, 2010; WHO-EURO, 2018b).
– Strengthening the communication capacities of vaccination services, including their engagement capacities with communities and their respected leaders, to ensure that messaging on vaccination is culturally and linguistically appropriate.
Five interventions have been identified to improve cultural competence in healthcare systems: a) programmes to recruit staff who reflect the cultural diversity of the community served; b) use of interpreter services or bilingual providers for patients with limited native language proficiency; c) training in cultural competence for healthcare providers; d) use of linguistically and culturally appropriate health education materials; and e) culturally specific healthcare settings (Anderson, 2003).
Medical schools in the United States have instituted cultural competence education in the undergraduate curriculum (Sears, 2012).
The project “Provision of training for first-line health professionals, social workers and law enforcement officers working at local level with migrants and refugees, and training of trainers” (TRAIN4M&H), funded by the European Commission, is another example of how positive attitudes can be improved and a holistic approach can be promoted in the work with migrants in European countries (Declich, 2020).
Providing early access to culturally appropriate health care and, in the absence of native speaker clinicians, interpretation services may be critical to ensuring provision of high-quality care for M&R populations, as shown by a collection of current public health interventions and practices in the WHO European region (WHO-EURO, 2018a).
The health service capacity to engage communities and implement targeted interventions to address specific reasons for under-immunisation is exemplified by a Swedish initiative in 2015-2016. Research on vaccine hesitancy determinants indicated that some parents within the Somali migrant community in Stockholm had concerns about the supposed (and disproven) link between MMR vaccination and autism and were reluctant to vaccinate their children. Competence among health professionals and communication to parents were strengthened: interventions targeting parents included “vaccine champion” and peer-topeer education projects, using educators from the Somali community. These key Somali informants conveyed information about vaccinations to the Swedish-Somali community, in the target group’s own language and considering cultural aspects (WHO-EURO, 2019).
A Collaborative Community aimed at facilitating productive and efficient communication between health departments and communities was created by the Washington State Department of Health during the COVID-19 pandemic. The COVID-19 Vaccine Implementation Collaborative engaged leaders from communities disproportionately impacted by the disease (including refugees, immigrants and migrants) with the aim of planning and reviewing Covid-19 vaccine implementation (Washington State Department of Health, 2021).
Pillar 4. Increased M&R health and vaccine literacy
– Establishing vaccine literacy education programmes and strategies to promote vaccine confidence and vaccine uptake among M&R (Crawshaw, 2021; Hanif, 2020).
– Offering health promotion educational interventions, with a community-based approach.
Vaccine literacy should consider both the individual’s level of health literacy and the complexities of the contexts within which people act (Kickbush, 2013).
Comprehensive, adequate, accessible and language & culturally friendly information and education materials on preventive measures tailored to migrants are not common (Fernandez-Gutiérrez, 2018), and even less so for vaccination, as a recent study conducted in Australia reported (Abdi, 2020).
An initiative tailored for asylum seekers in Germany showed that the provision of information material in various languages and via interpreters, alongside information sessions with local healthcare staff, resulted in a substantial increase in vaccination uptake among children and adolescents (Brockmann, 2016).
Recent considerations for COVID-19 vaccine uptake among Asian communities in the United Kingdom (Hanif, 2020) indicate that social mobilisation, community outreach and community engagement are strategies to pursue.
Pillar 5. Monitoring progress of inclusive vaccinations, based on a health equity perspective
– Setting up strategic goals, targets and indicators for national vaccination plans, to allow for monitoring of progress and of impact, based on a health equity perspective (Figure 3).
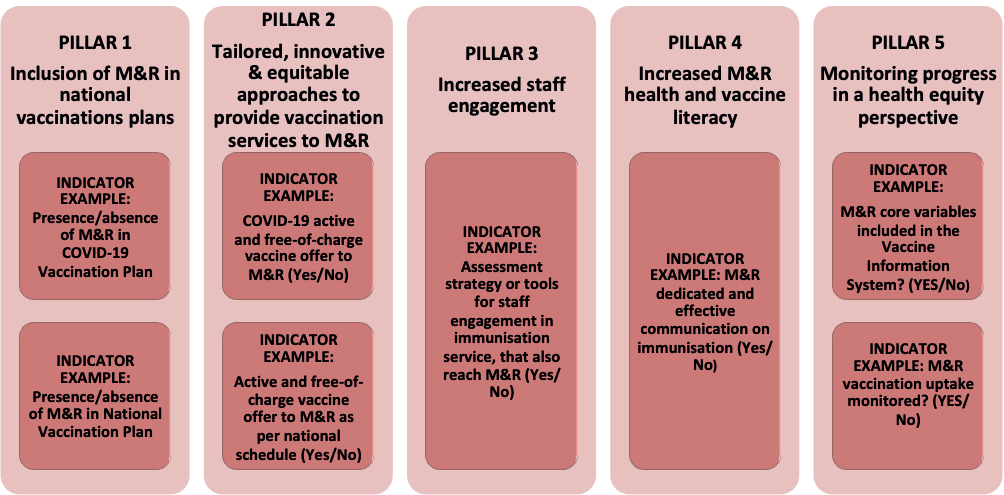
Figure 3: Key pillars for M&R inclusion in prevention and vaccination services and examples of monitoring indicators
– Setting up or expanding immunisation information systems to monitor vaccination coverage, with appropriate disaggregation by key social determinants of health. The core variables recommended in relation to the migration status are country of birth; country of citizenship; month and year of arrival; and country of birth of both parents. Integration of a second set of recommended variables will allow further disaggregation of health data by subgroups of migrants: reasons for migration; knowledge of official language(s) of host country; ever resided abroad; and legal status (WHO-EURO, 2021).
– Setting an appropriate vaccination coverage target also for M&R, at least for diseases targeted for elimination or eradication (e.g., polio and measles).
RECOMMENDATIONS FOR THE G20
In this context, with a view to bringing these pillars into the international health agenda and to support and catalyse national level efforts, G20 countries should therefore collectively and publicly commit to:
– Including M&Rs in fully funded, inclusive national COVID-19 response plans: in particular, vaccinations plans should prioritise subgroups of migrants who are at significantly higher risk due to their living conditions and/or their legal status, in line with Stage II of the WHO SAGE Roadmap (WHO, 2020b);
– Supporting inclusive COVID-19 vaccination plans outside theG20, by financially supporting Covax; and by endorsing the WHO SAGE prioritisation roadmap which locates subgroups of M&R as priority groups for phase II immunisation;
– Including M&R in their national vaccination plans, including life-course vaccination programmes beyond the COVID-19 epidemic;
– Increasing multilateral dialogue among countries to ensure cross-border consistency of guidelines and the interoperability of immunisation records;
– Monitoring disparities and measure impact: agree on migrant-sensitive indicators in vaccination pillars at national and regional levels, as indicated above; agree on internationally coordinated data disaggregation, including by migration status, in surveillance and health information systems, and specifically in vaccination systems;
– Investing in G20 and partner countries’ health systems in terms of the accessibility, cultural competence, institutional health literacy, proximity and outreach capacity of vaccination services, in order to reach M&R, engage them in vaccination services and increase vaccination coverage;
– Acknowledging the need for undocumented migrants to access vaccine services during and beyond the current COVID-19 pandemic, in the interest of both individual and public health: where formal entitlements are not already in place, the G20 may recommend temporary exceptions;
– Recognising that access to COVID-19 vaccine and, to the extent possible, to other vaccines, should be free of charge for everyone, including M&Rs, in both low-, middleand high-income countries.
CONCLUSION
Ensuring rapid and universal access to COVID-19 vaccines is an unmissable opportunity not just to maximise their effectiveness, but also to set up, test and implement new approaches in primary prevention and vaccination services that are effective and replicable for all other vaccine preventable diseases, fostering equity in health and protecting public health.
“Migrant and displaced communities regardless of their legal status urgently need to be explicitly and proactively included in vaccination plans. This action not only recognises the interdependence between migrant health and public health but also offers a crucial opportunity to strengthen the dissemination of vital public health information to this excluded group and engage them in health systems to address wider protracted disparities” (Al-Oraibi, 2021).
Accordingly, we suggest that the G20 include the following wording in their Final Communiqué:
Ensure that COVID-19 vaccine coverage is equitable among and within countries to prevent the occurrence of under-immunised population groups, such as M&R.
Extend this approach beyond the current pandemic and the COVID-19 vaccine in order to enhance preparedness to present and future health threats.
Include M&R-specific strategic goals, targets and indicators in the national vaccination plans based on a health equity and public health perspective.
Specifically, agree on and roll-out a minimum set of health indicators to allow for monitoring of immunisation progresses and impact among socially vulnerable groups, with specific reference to M&R, to be collected and compared among G20 countries and beyond.
APPENDIX
The European and Global Vaccination Plans contain reference to equity in immunisation and consideration of vulnerable groups and marginalised populations.
- The Council of the European Union, in its Recommendation on Strengthened Cooperation against Vaccine-Preventable Diseases, advocates that the member states facilitate access to national vaccination services, by: (a) simplifying and broadening opportunities to offer vaccination, leveraging community based providers; and (b) ensuring targeted outreach to the most vulnerable groups, including socially excluded groups, so as to bridge inequalities and gaps in vaccination coverage (European Commission, 2018).
- The World Health Assembly in August 2020 endorsed a new global vision and strategy, called the Immunization Agenda 2030 (IA2030) A Global Strategy to Leave No One Behind, to address challenges over the next decade and save over 50 million lives. IA2030 envisions a world where everyone, everywhere, at every age, fully benefits from vaccines to improve health and well-being. It aims to maintain hard-won gains in immunisation, recover from the disruptions caused by COVID-19, and achieve even more by leaving no one behind, in any situation or at any stage of life. In particular, it states that if all people are to access immunisation services, vaccines must be delivered to areas that are isolated geographically, culturally, socially or otherwise and to marginalised populations such as displaced people and migrants and those affected by conflict, political instability and natural disasters (WHO, 2020c).
NOTES
1 Although consolidated glossaries exist (e.g. IOM, 2019), in the present policy brief we are not providing a specific definition of “migrants and refugees”, as these terms are highly context and migration policy dependent. Moreover, the complexity inherent in the relationship between migration and health is known (The Lancet, 2006). Our perspective here will refer mainly to the European region, although experiences from other countries are included, too.
REFERENCES
Abdi, Ikram; Bernice Murphy; and Holly Seale (2020), “Evaluating the Health Literacy Demand and Cultural Appropriateness of Online Immunisation Information Available to Refugee and Migrant Communities in Australia” in Vaccine, Vol. 38, No. 41, 22 September, pp. 6410-6417, https://doi.org/10.1016/j.vaccine.2020.07.071
Al-Oraibi, Amani; Christopher A Martin; Osama Hassan; Kolitha Wickramage; Laura B. Nellums; and Manish Pareek (2021), “Migrant Health Is Public Health: A Call for Equitable Access to COVID-19 Vaccines” in The Lancet Public Health, Vol. 6, No. 3 (March), p. 144, https://doi.org/10.1016/S2468-2667(21)00031-1
Anderson, Laurie M.; Susan C. Scrimshaw; Mindy T. Fullilove; Jonathan E. Fielding; Jaques Normand; and Task Force on Community Preventive Services (2003), “Culturally Competent Healthcare Systems. A Systematic Review” in American Journal of Preventive Medicine, Vol. 24, No. 3 (April), pp. 68-79, https://doi.org/10.1016/S0749-3797(02)00657-8
Bartovic, Jozef; Siddharta Sankar Dat ta; Santino Severoni; and Veronika D’Anna (2021), “Ensuring Equitable Access to Vaccines for Refugees and Migrants During the COVID-19 Pandemic”, in Bulletin of the World Health Organization, Vol. 99, pp. 3-3A, http://dx.doi.org/10.2471/BLT.20.267690
Brockmann, Stefan O.; Stephanie Wjst; Ursula Zelmer; Stefanie Carollo; Mirjam Schmid; Gottfried Roller; and Martin Eichner (2016), “ÖGD-Initiative zur Ver besserung der Durchimpfung bei Asylsuchenden – Public Health Initiative for Improved Vaccination for Asylum Seek ers”, in Bundesgesundheitsblatt – Gesundheitsforschung – Gesundheitsschutz, Vol. 59 (12 April), pp. 592-598, https://doi.org/10.1007/s00103-016-2335-6
Charania, Nadia A.; Nina Gaze; Janice Y. Kung; and Stephanie Brooks (2019), “Vaccine-Preventable Diseases and Immunisation Coverage among Migrants and Non-Migrants Worldwide: A Scoping Review of Published Literature, 2006 to 2016”, in Vaccine, Vol. 37, No. 20 (6 May), pp. 2661-2669, https://doi.org/10.1016/j.vaccine.2019.04.001
Charania, Nadia A.; Nina Gaze; Janice Y. Kung; and Stephanie Brooks (2020), “Interventions to Reduce the Burden of Vaccine-Preventable Diseases Among Migrants and Refugees Worldwide: A Scoping Review of Published Literature, 2006-2018”, in Vaccine, Vol. 38, No. 46 (27 October), https://doi.org/10.1016/j.vaccine.2020.09.054
Conferenza Permanente per i rapporti tra lo Stato, le Regioni e le Province autonome di Trento e Bolzano (2012), Accordo ai sensi dell’articolo 4 del decreto legislativo 28 agosto 1997, n. 281, tra il Governo, le Regioni e le Province autonome di Trento e Bolzano sul documento recante: «Indicazioni per la corretta applicazione della normativa per l’assistenza sanitaria alla popolazione straniera da parte delle Regioni e Province autonome (Rep. Atti n. 255/CSR), 20 December, https://www.gazzettaufficiale.it/eli/id/2013/02/07/13A00918/sg
Alison F. Crawshaw, Anna Deal, Kieran Rustage, Alice S. Forster, Ines Campos-Matos, Tushna Vandrevala, Andrea Würz, Anastasia Pharris, Jonathan Suk, John Kinsman, Charlotte Deogan, Anna Miller, Silvia Declich, Chris Greenaway, Teymur Noori and Sally Hargreaves, “What Must Be Done to Tackle Vaccine Hesitancy and Barriers to COVID-19 Vaccination in Migrants?”, in Journal of Travel Medicine, taab048 (26 March 2021), https://doi.org/10.1093/jtm/taab048
De Vito, Elisabetta; Paolo Parente; Chiara de Waure; Andrea Poscia; and Walter Ricciardi (2017), A Review of Evidence on Equitable Delivery, Access and Utilization of Immunization Services for Migrants and Refugees in the WHO European Region, Copenhagen, WHO Regional Office for Europe (Health Evidence Network Synthesis Report No. 53), https://www.euro.who.int/__data/assets/pdf_file/0005/351644/HEN53.pdf
Declich, Silvia; Giulia De Ponte; Maria Laura Russo; Giulia Marchetti; Maria Grazia Dente; Ornella Punzo; and Maurizio Marceca (2020), “Turning Constraints into Resources: The Experience of TRAIN4M&H Training Program on Migrants’ Health”, in European Journal of Public Health, Vol. 30, No. Supplement 5 (September), p. v62, https://doi.org/10.1093/eurpub/ckaa165.164
Dobson, Andrew P.; Stuart L. Pimm; Lee Hannah; Les Kaufman; Jorge A. Ahumada; Amy W. Ando; Aaron Bernstein; Jonah Busch; Peter Daszak; Jens Engelmann; Margaret F. Kinnaird; Binbin V. Li; Ted Loch-Temzelides; Thomas Lovejoy; Katarzyna Nowak; Patrick R. Roehrdanz; and Mariana M. Vale (2020), “Ecology and Economics for Pandemic Prevention”, in Science, Vol. 369, No. 6502 (24 July), pp. 379-381, https://science.sciencemag.org/content/369/6502/379/tab-pdf
European Centre for Disease Prevention and Control (ECDC) (2020), COVID-19 Vaccination and Prioritisation Strategies in the EU/EEA, Stockholm (technical report), https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-vaccination-and-prioritisation-strategies.pdf
European Centre for Disease Prevention and Control (ECDC) (2021), Reducing COVID-19 Exposure and Strengthening
Vaccine Uptake among Migrant Populations in the EU/EEA Countries, Stockholm (technical report) https://www.ecdc.europa.eu/en/publications-data/covid-19-migrants-reducing-transmission-and-strengthening-vaccine-uptake
European Commission (2018), Council Recommendation of 7 December 2018 on Strengthened Cooperation Against Vaccine-Preventable Diseases, 14152/1/18 REV 1 – 2018/0115(NLE), https://ec.europa.eu/health/sites/health/files/vaccination/docs/14152_2018_en.pdf
Fang, Hai; Li Yang; Huyang Zhang; Chenyang Li, Liankui Wen; Li Sun; Kara Hanson; and Qingyue Meng (2017), “Strengthening Health System to Improve Immunization for Migrants in China”, in International Journal for Equity in Health, Vol. 16, No. 19 (July), https://doi.org/10.1186/s12939-016-0504-8
Fernández-Gutiérrez, Martina; P. BasSarmiento; Maria J. Albar-Marín; Olga Paloma-Castro; and J. M. Romero-Sánchez (2017), “Health Literacy Interventions for Immigrant Populations: A Systematic Review”, in International Nursing Review, Vol. 65, No. 1 (27 April), pp. 54-64, https://doi.org/10.1111/inr.12373
Giambi, Cristina; Martina Del Mans; Giulia Marchetti; Kate Olsson; Karam Adel Ali; and Silvia Declich (2019), “Venice Survey Working Group. Immunisation of Migrants In EU/EEA Countries: Policies and Practices”, in Vaccine, Vol. 37, No. 36 (8 July), pp. 5439-5451, https://doi.org/10.1016/j.vaccine.2019.06.068
Hanif, Wasim; Sarah N. Ali; Kiran Patel; and Kamlesh Khunti (2020), “Cultural Competence in COVID-19 Vaccine Rollout”, in BMJ, Vol. 371, No. m4845 (18 December), https://doi.org/10.1136/bmj.m4845
Hu, Yu; Shuying Luo; Xuewen Tang; Linqiao Lou; Yaping Chen; and Jing Guo (2015), “Comparative Assessment of Immunization Coverage of Migrant Children between National Immunization Program Vaccines and Non-National Immunization Program Vaccines in East China”, in Human Vaccines & Immunotherapeutics, Vol. 11, No. 3, pp. 761-768, https://doi.org/10.1080/21645515.2015.1012015
International Organization for Migration (IOM) (2019), International Migration Law Glossary on Migration, Geneva, IOM (No. 34), https://publications.iom.int/system/files/pdf/iml_34_glossary.pdf
Kickbusch, Ilona; Jürgen M. Pelikan; Franklin Apfel; and Agis D. Tsouros (eds) (2013), Health Literacy. The Solid Facts, Copenhagen, World Health Organization (WHO) Regional Office for Europe, pp. 19-21, https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf
Ministry of Health (MoH) of Singapore (2021), Covid-19 Vaccination Brought Forward for All Seniors; Extended to Essential Services Personnel and Higher Risk Groups, 8 March, https://www.moh.gov.sg/news-highlights/details/covid-19-vaccination-brought-forward-for-all-seniorsextended-to-essential-services-personnel-and-higher-risk-groups
Mitchell, Tarissa; Michelle Weinberg; Drew L. Posey; and Martin Cetron (2019), “Immigrant and Refugee Health: A Centers for Disease Control and Prevention Perspective on Protecting the Health and Health Security of Individuals and Communities During Planned Migrations”, in Pediatric Clinics of North America, Vol. 66, No. 3, pp. 549-560, https://pubmed.ncbi.nlm.nih.gov/31036234/
PICUM (2021), The COVID-19 Vaccines and Undocumented Migrants: What Are European Countries Doing?, March, https://picum.org/covid-19-vaccines-undocumented-migrants-europe/
Public Health Agency (PHA) of Canada (2021), Canadian Immunization Guide,26March, https://www.canada.ca/en/publichealth/services/canadian-immunizationguide.html
Ravensbergen, Sofanne J.; Laura B. Nellums; Sally Hargreaves; Ymkje Stienstra; Jon S. Friedland; and ESGITM Working Group on Vaccination in Migrants (2019), “National Approaches to the Vaccination of Recently Arrived Migrants In Europe: A Comparative Policy Analysis across 32 European Countries”, in Travel Medicine and Infectious Disease, Vol. 27, pp. 33-38, https://www.sciencedirect.com/science/article/pii/S1477893918303661?via%3Dihub
Riccardo, Flavia; Maria Grazia Dente; Mira Kojouharova; Massimo Fabiani; Valeria Alfonsi; Anna Kurchatova; Nadezhda Vladimirova; and Silvia Declich (2012), “Migrant’s Access to Immunization in Mediterranean Countries”, in Health Policy, Vol. 105, No. 1 (April), pp. 17-24, https://doi.org/10.1016/j.healthpol.2012.02.004
Sears, Karen P. (2012), “Improving Cultural Competence Education: The Utility of an Intersectional Framework”, in Medical Education, Vol. 46, No. 6 (June), pp. 545-551, https://doi.org/10.1111/j.13652923.2011.04199.x
The Lancet (2006), “Migration and Health: A Complex Relation”, in Lancet, Vol. 368, No. 9541 (23 September), p. 1039, https://doi.org/10.1016/S0140-6736(06)69423-3
Tosti, Maria Elena; Maurizio Marceca; Erica Eugeni; Franca D’Angelo; Salvatore Geraci; Silvia Declich; Maurella Della Seta; Luigina Ferrigno; Rosalia Marrone; Chiara Pajno; Scilla Pizzarelli; Annalisa Rosso; Giulia De Ponte; Concetta Mirisola; and Giovanni Baglio (2021), “Health Assessment for Migrants and Asylum Seekers upon Arrival and While Hosted in Reception Centres: Italian Guidelines”, in Health Policy, Vol.123, No. 3 (March), pp. 393-405, https://doi.org/10.1016/j.healthpol.2020.12.010
UNHCR (2021), Rwanda Vaccinates Refugees and Asylum-Seekers against COVID-19, 12 March, https://www.unhcr.org/news/press/2021/3/604b63ed4/rwandavaccinates-refugees-asylum-seekersagainst-covid-19.html
Washington State Department of Health (2021), COVID-19 Vaccine Implementation Collaborative, March, https://www.doh.wa.gov/Emergencies/COVID19/VaccineInformation/Engagement/Collaborative
Wilson, Lindsay; Taylor Rubens-August son; Malia Murphy; Cindy Jardine; Natasha Crowcroft; Charles Hui; and Kumanan Wilson (2018), “Barriers to Immunization among Newcomers: A Systematic Review”, in Vaccine, Vol. 36, No. 8 (14 February), pp. 1055-1062, https://doi.org/10.1016/j.vaccine.2018.01.025
World Bank Group (WB) (2020), Global Economic Prospects, Data Bank, January, https://databank.worldbank.org/source/global-economic-prospects
World Health Organization (WHO) (ed) (2010), Health of Migrants: The Way Forward: Report of a Global Consultation. Madrid, Spain, 3-5 March 2010, Geneva, WHO, http://www.who.int/hac/events/consultation_report_health_migrants_colour_web.pdf
World Health Organization (WHO) (2020a), WHO SAGE Values Framework for the Allocation and Prioritization of COVID-19 Vaccination, 14 September, https://apps.who.int/iris/handle/10665/334299
World Health Organization (WHO) (2020b), WHO SAGE Roadmap for Prioritizing Uses of COVID-19 Vaccines in the Context of Limited Supply, Geneva, WHO, 13 November, https://www.who.int/publications/i/item/who-sage-roadmap-forprioritizing-uses-of-covid-19-vaccines-inthe-context-of-limited-supply
World Health Organization (WHO) (2020c), Implementing the Immunization Agenda 2030: Draft Framework for Action through Coordinated Planning, Monitoring & Evaluation, and Ownership & Accountability, 25 November, https://www.who.int/publications/m/item/implementing-the-immunization-agenda-2030
World Health Organization Regional Office for Europe (WHO-EURO) (2018a), Health of Refugees and Migrants Regional Situation Analysis, Practices, Experiences, Lessons Learned and Ways Forward, WHO European Region, https://www.who.int/migrants/publications/EURO-report.pdf?ua=1
World Health Organization Regional Office for Europe (WHO-EURO) (2018b), Report on the Health of Refugees and Migrants in the WHO European Region: No Public Health without Refugee and Migrant Health, Copenhagen, WHO Regional Office for Europe, https://apps.who.int/iris/bitstream/handle/10665/311347/9789289053846-eng.pdf?sequence=1&isAllowed=y
World Health Organization Regional Office for Europe (WHO-EURO) (2019), Delivery of Immunization Services for Refugees and Migrants: Technical Guidance, Copenhagen, WHO Regional Office for Europe, https://apps.who.int/iris/handle/10665/326924
World Health Organization Regional Officer for Europe (WHO-EURO) (2021), Collection and Integration of Data on Refugee and Migrant Health in the WHO European Region: Policy Brief, https://apps.who.int/iris/bitstream/handle/10665/338803/WHO-EURO-2021-1864-41615-56852-eng.pdf?sequence=1&isAllowed=y